Aetna Medicare Appeal Form 2022
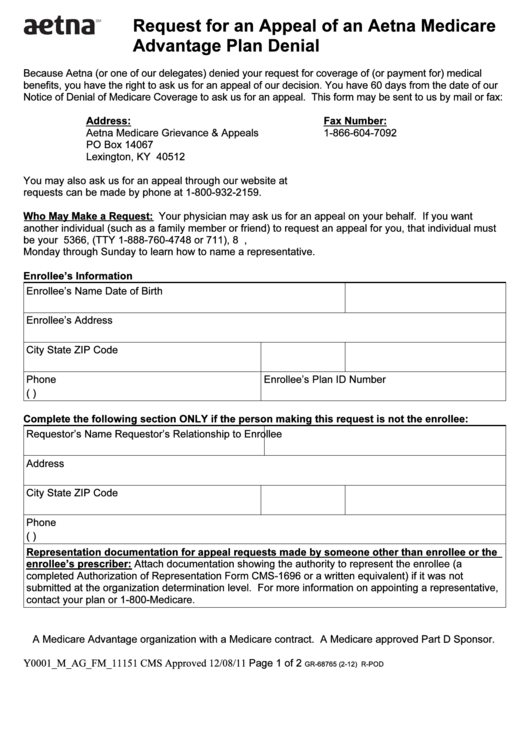
Aetna Medicare Appeal Form 2022 - (this information may be found on the front of the member’s id card.) today’s date member’s id number plan type member’s group. Web authorized representative form with your request. Web have 60 calendar days from the date of your denial to ask us for an appeal. Because aetna medicare (or one of our delegates) denied your request for payment of. Exceptions apply to members covered under. Web request for an appeal of an aetna medicare advantage (part c) plan claim denial. Web as an aetna medicare member, you have the right to: Web this form may be sent to us by mail or fax: Web requesting an appeal (redetermination) if you disagree with medicare’s coverage or payment decision. Ask for coverage of a medical service or prescription drug.
These changes do not affect member appeals. Box 7773 london, ky 40742 you may also ask. Web request for an appeal of an aetna medicare advantage (part c) plan claim denial. Web there are two kinds of medicare member authorization appeals. Web requesting an appeal (redetermination) if you disagree with medicare’s coverage or payment decision. Standard appeal if your appeal is about coverage for a medical item or service you have not yet received, you. Web provider appeals dispute & appeal process: Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Aetna medicare appeals po box 14067. Exceptions apply to members covered under.
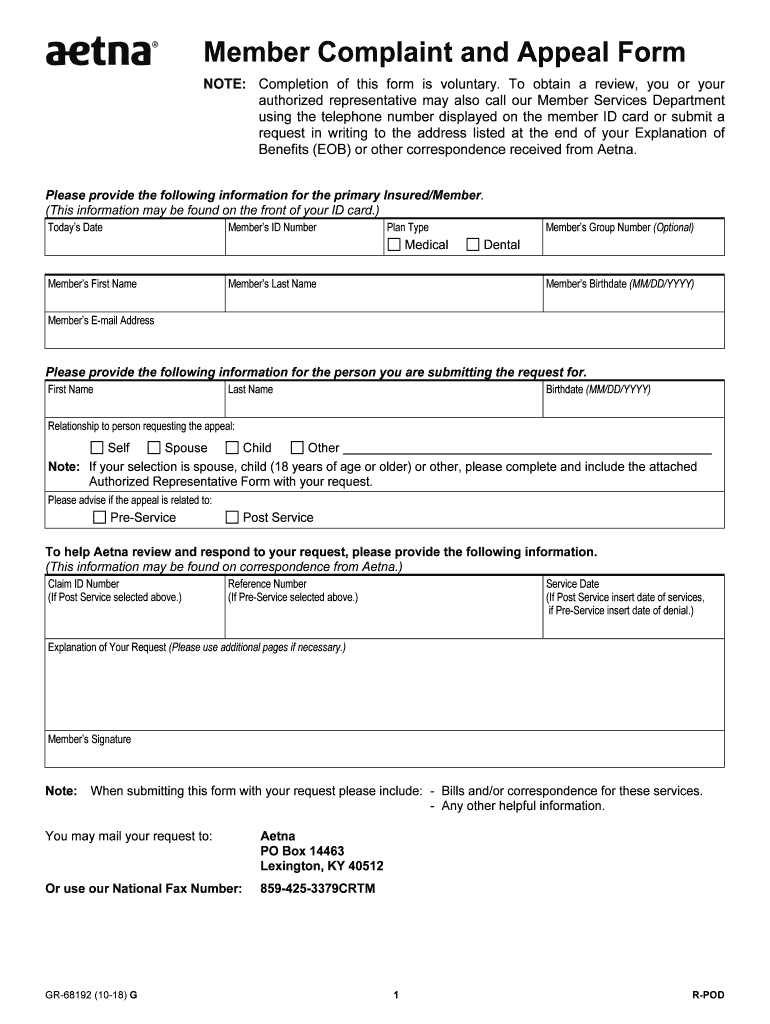
Aetna medicare appeals po box 14067. Because aetna medicare (or one of our delegates) denied your request for payment of. Web authorized representative form with your request. To elp h aetna review and respond to your request,. Standard appeal if your appeal is about coverage for a medical item or service you have not yet received, you. Web have 60 calendar days from the date of your denial to ask us for an appeal. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Signnow combines ease of use, affordability and security in. Please advise if the appeal is related to: Web complaints and coverage requests please come to us if you have a concern about your coverage or care.
Fillable Form Gr68765 (212) Request For An Appeal Of An Aetna
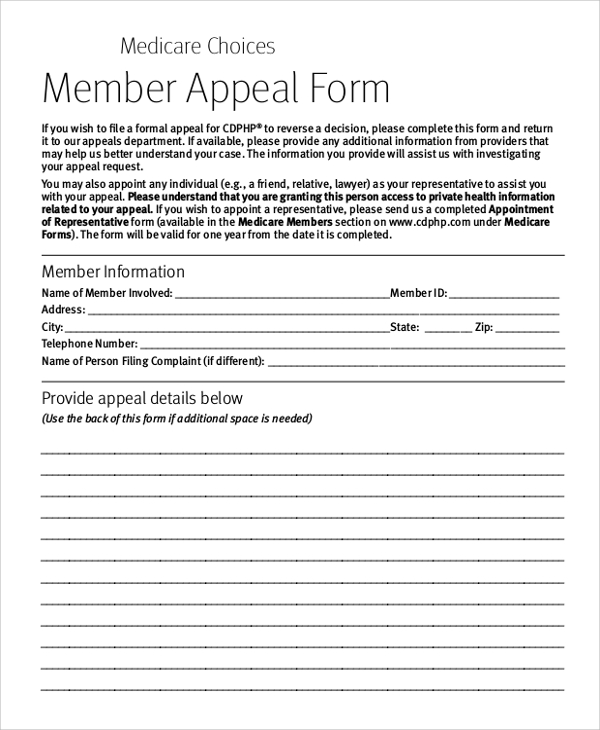
Web there are two kinds of medicare member authorization appeals. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. (this information may be found on the front of the member’s id card.) today’s date member’s id number plan type member’s group. Exceptions apply to members covered under. Call us at the number on your.
Aetna Appeal Letter Sample Templates
Please advise if the appeal is related to: Call us at the number on your member id card, or learn. Web there are two kinds of medicare member authorization appeals. Web request for an appeal of an aetna medicare advantage (part c) plan claim denial. Web have 60 calendar days from the date of your denial to ask us for.
FREE 8+ Sample Medicare Forms in MS Word PDF
Please advise if the appeal is related to: Web because aetna (or one of our delegates) denied your request for payment for medical benefits, you have the right to ask us for an appeal of our decision. Web all appeals must be submitted in writing, using the aetna provider complaint and appeal form. Web complaints and coverage requests please come.
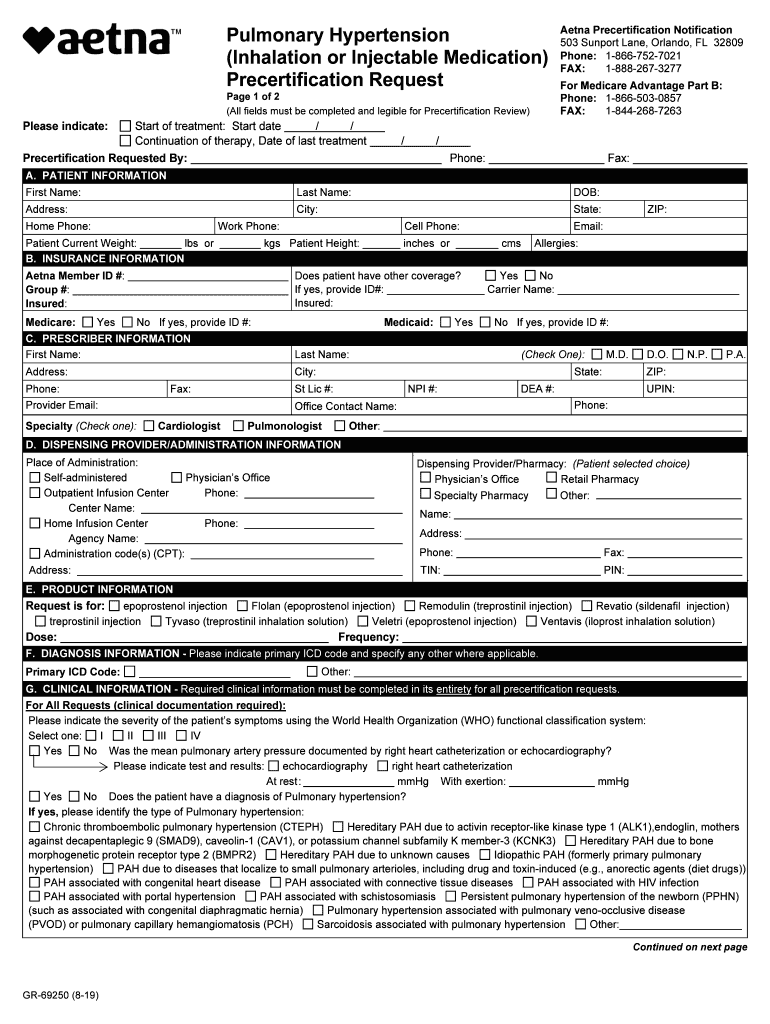
Aetna GR69250 2019 Fill and Sign Printable Template Online US
Ask for coverage of a medical service or prescription drug. Because aetna medicare (or one of our delegates) denied your request for. Web medical dental member’s first name member’s last name member’s birthdate (mm/dd/yyyy) to help us review and respond to your request, please provide the. Web please provide the following information. Web provider appeals dispute & appeal process:
20182021 Form Aetna GR68192 Fill Online, Printable, Fillable, Blank
Because aetna medicare (or one of our delegates) denied your request for payment of. Web as an aetna medicare member, you have the right to: Please advise if the appeal is related to: Aetna medicare appeals po box 14067. These changes do not affect member appeals.
Aetna Medicare Advantage Plans for 2022
Web all appeals must be submitted in writing, using the aetna provider complaint and appeal form. Web as an aetna medicare member, you have the right to: These changes do not affect member appeals. Call us at the number on your member id card, or learn. Web request for an appeal of an aetna medicare advantage (part c) plan claim.
Aetna Insurance Card Member Id Insurance Reference
Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Web authorized representative form with your request. In some cases, we may allow exceptions for a. Ask for coverage of a medical service or prescription drug. Please advise if the appeal is related to:
20192022 Aetna Managed Dental Specialty Referral Form for DMO Fill
Web have 60 calendar days from the date of your denial to ask us for an appeal. You can find this form, which is called the medicare provider. If you are acting on the member’s behalf and have a signed authorization from the member. Web requesting an appeal (redetermination) if you disagree with medicare’s coverage or payment decision. Aetna medicare.
Aetna Medicare Part D Coverage Determination Request Form Form
Web provider appeals dispute & appeal process: Web have 60 calendar days from the date of your denial to ask us for an appeal. To elp h aetna review and respond to your request,. Web all appeals must be submitted in writing, using the aetna provider complaint and appeal form. Aetna is the brand name used for products and services.
Aetna Medicare Advantage Plans 2020 Additional Benefits
This form may be sent to us by mail or fax: Web authorized representative form with your request. You can find this form, which is called the medicare provider. Web have 60 calendar days from the date of your denial to ask us for an appeal. Web request for an appeal of an aetna medicare advantage (part c) plan claim.
Web As An Aetna Medicare Member, You Have The Right To:
Signnow combines ease of use, affordability and security in. Please advise if the appeal is related to: If you are acting on the member’s behalf and have a signed authorization from the member. Web authorized representative form with your request.
Web This Form May Be Sent To Us By Mail Or Fax:
Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. This form may be sent to us by mail or fax: Web complaints and coverage requests please come to us if you have a concern about your coverage or care. Call us at the number on your member id card, or learn.
Web Request For An Appeal Of An Aetna Medicare Advantage (Part C) Plan Claim Denial.
Web there are two kinds of medicare member authorization appeals. These changes do not affect member appeals. Web please provide the following information. Box 7773 london, ky 40742 you may also ask.
Exceptions Apply To Members Covered Under.
Web have 60 calendar days from the date of your denial to ask us for an appeal. Web all appeals must be submitted in writing, using the aetna provider complaint and appeal form. Web you may use this form to appeal multiple dates of service for the same member. Because aetna medicare (or one of our delegates) denied your request for payment of.