Caremark Prior Auth Form
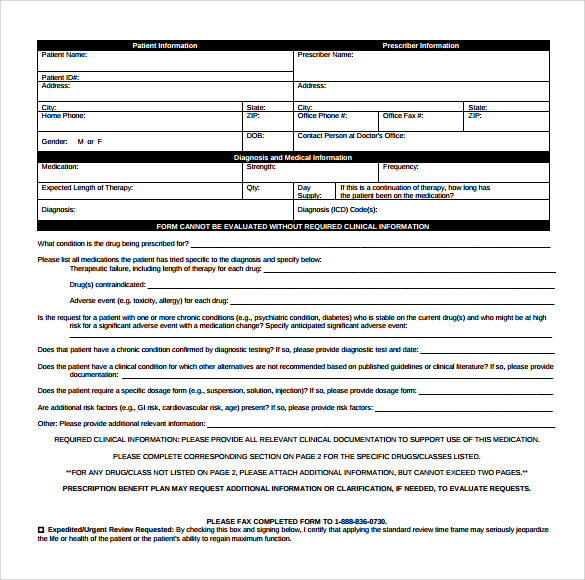
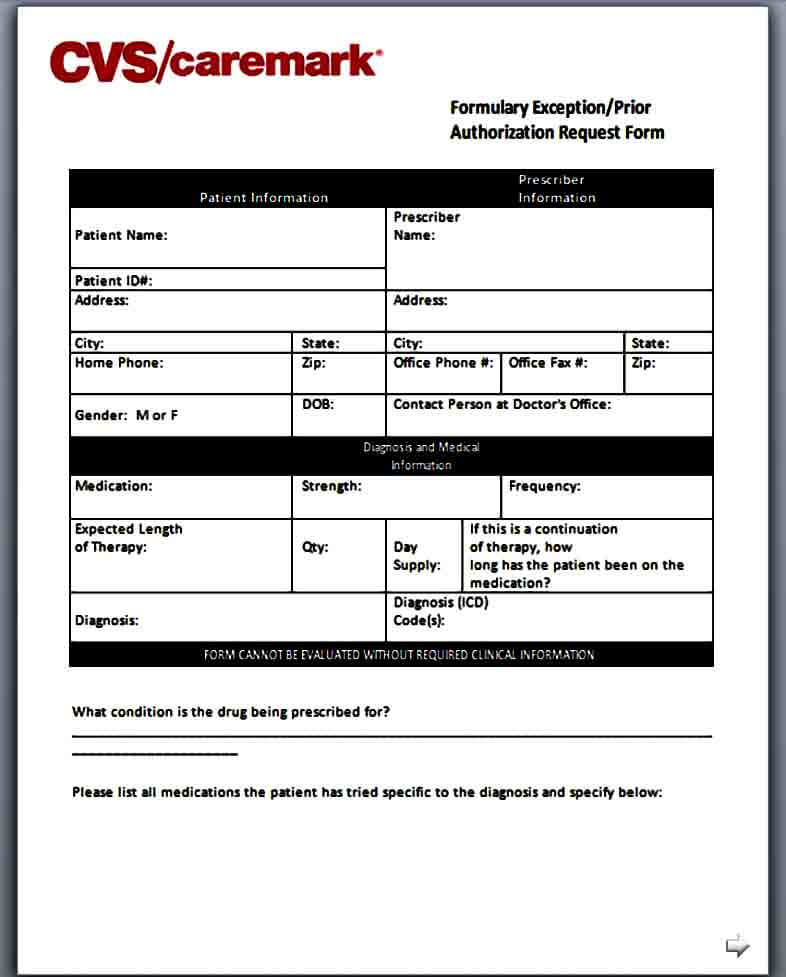
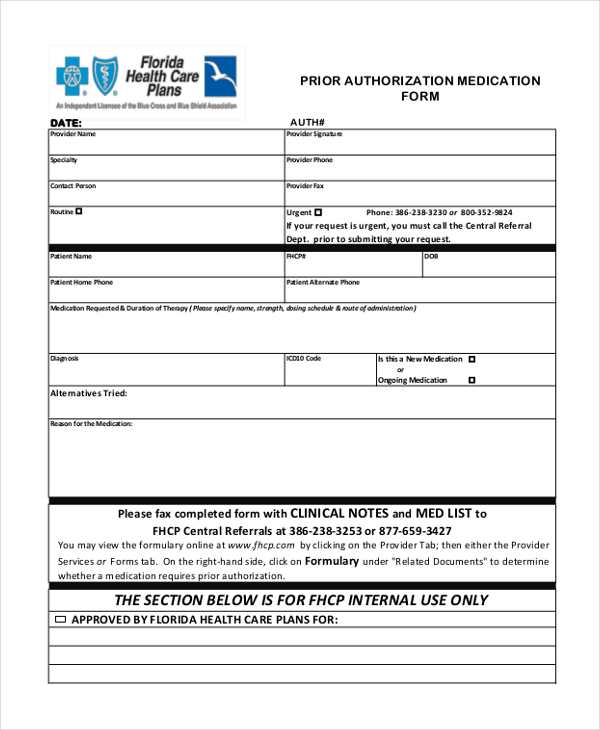
Caremark Prior Auth Form - Use the arrows next to each medication name to expand your selection. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Web formulary exception/prior authorization request form expedited/urgent review requested: Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you. Web download, review and print the prior approval form for the requested medication. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. Here is what your colleagues are. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. Web formulary exception/prior authorization request form patient information prescriber information patient name:
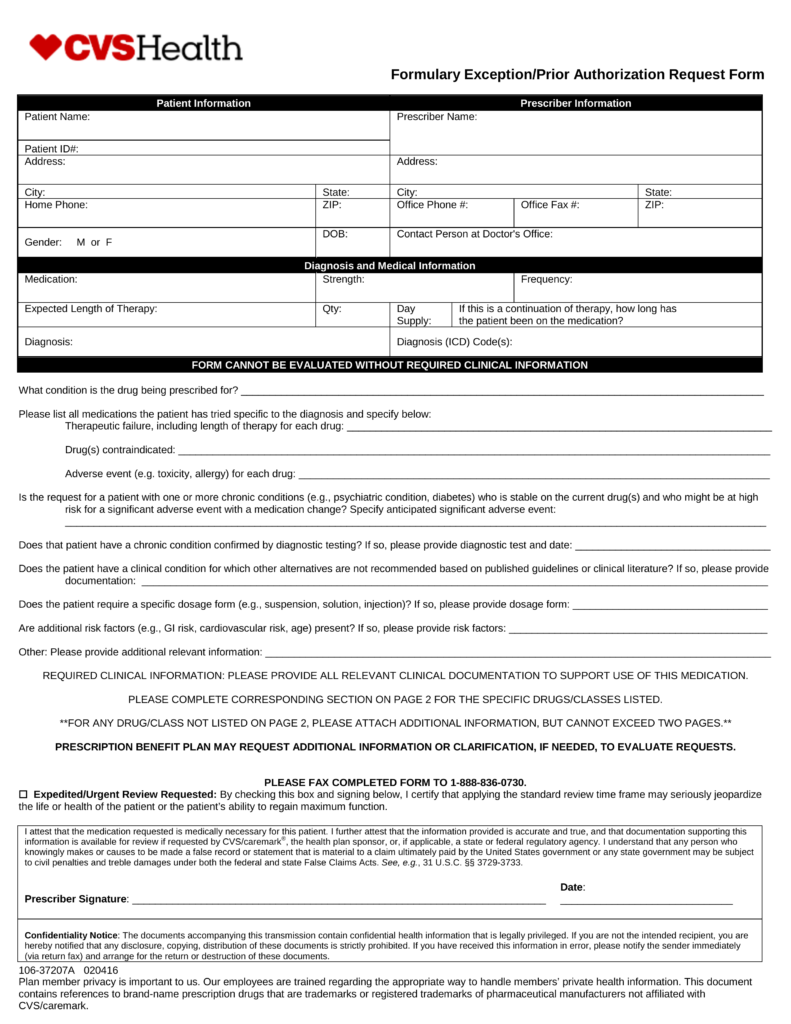
By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web cvs caremark has made submitting pas easier and more convenient. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. We've partnered with covermymeds ® and surescripts ®, making it easy for you to access electronic prior authorization (epa) via the epa vendor of your choice. Here is what your colleagues are. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. Web download, review and print the prior approval form for the requested medication.
Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. Select the starting letter of the name of the medication to begin. Web cvs caremark has made submitting pas easier and more convenient. Web select the appropriate cvs caremark form to get started. Use the arrows next to each medication name to expand your selection. Web formulary exception/prior authorization request form expedited/urgent review requested: Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web download, review and print the prior approval form for the requested medication. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests.
Template Caremark Prior Authorization Form Mous Syusa
A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Web download, review and print the prior approval form for the requested medication. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. A cvs/caremark prior authorization form is to be.
cvscaremarkpriorauthorizationform600x800 Free Job Application Form
Web select the appropriate cvs caremark form to get started. Web formulary exception/prior authorization request form expedited/urgent review requested: Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you. Select the starting letter of the name of the medication to begin..
CVS Caremark 10637207A 20192021 Fill and Sign Printable Template
A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Use the arrows next to each medication name to expand your selection. Web prior authorization forms pa forms for physicians when a pa is.
Cvs Caremark Prior Auth Form Pdf
Web formulary exception/prior authorization request form patient information prescriber information patient name: Here is what your colleagues are. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Cvs caremark prior authorization (pa) tools.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Web cvs caremark has made submitting pas easier and more convenient. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web formulary exception/prior authorization request form patient information prescriber information patient name: Web download, review and print the prior approval form for.
Template Caremark Prior Authorization Form Mous Syusa
Here is what your colleagues are. We've partnered with covermymeds ® and surescripts ®, making it easy for you to access electronic prior authorization (epa) via the epa vendor of your choice. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to.
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you. Web formulary exception/prior authorization request form expedited/urgent review requested: Web updated june 02,.
Cvs Caremark Appeal Form Fill Out and Sign Printable PDF Template
Here is what your colleagues are. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Covermymeds is.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Web updated june 02, 2022. Some automated decisions may be communicated in less than 6 seconds! Select the starting letter of the name of the medication to begin. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. By checking this box.
Info Caremark Epa Form Fill Out and Sign Printable PDF Template signNow
Web select the appropriate cvs caremark form to get started. Use the arrows next to each medication name to expand your selection. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Web updated june 02, 2022.
Web Updated June 02, 2022.
A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Web formulary exception/prior authorization request form patient information prescriber information patient name: Some automated decisions may be communicated in less than 6 seconds!
Web Select The Appropriate Cvs Caremark Form To Get Started.
We've partnered with covermymeds ® and surescripts ®, making it easy for you to access electronic prior authorization (epa) via the epa vendor of your choice. Here is what your colleagues are. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests.
Web Cvs Caremark Has Made Submitting Pas Easier And More Convenient.
Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate.
By Checking This Box And Signing Below, I Certify That Applying The Standard Review Time Frame May Seriously Jeopardize The Life Or Health Of The Patient Or The Patient’s Ability To Regain Maximum Function.
Web download, review and print the prior approval form for the requested medication. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs.