Hmsa Prior Authorization Form
Hmsa Prior Authorization Form - Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans: Web standard request for medicare and medicaid plans: This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Hmsa medical management department p. Decisions & notification are made within 15calendar days* expedited request (md,. Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date: To make an appropriate determination, providing the most accurate diagnosis for the use of the _ patient information last name first name phone number gender m f date of birth member id # (if known): Web utilization management (um) department prior authorization request phone number: Contact name (first, last) member.
Web utilization management (um) department prior authorization request phone number: This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Fast pass providers aren’t required to request prior authorization. This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Decisions & notification are made within 15calendar days* expedited request (md,. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. Contact name (first, last) member. _ patient information last name first name phone number gender m f date of birth member id # (if known): To make an appropriate determination, providing the most accurate diagnosis for the use of the Hmsa medical management department p.
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date: Web standard request for medicare and medicaid plans: _ patient information last name first name phone number gender m f date of birth member id # (if known): This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Contact name (first, last) member. Web utilization management (um) department prior authorization request phone number:
REQUEST FOR MEDICAL AUTHORIZATION in Word and Pdf formats
Hmsa medical management department p. To make an appropriate determination, providing the most accurate diagnosis for the use of the Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans: Web utilization management (um) department prior authorization request phone number: Contact name (first, last) member.
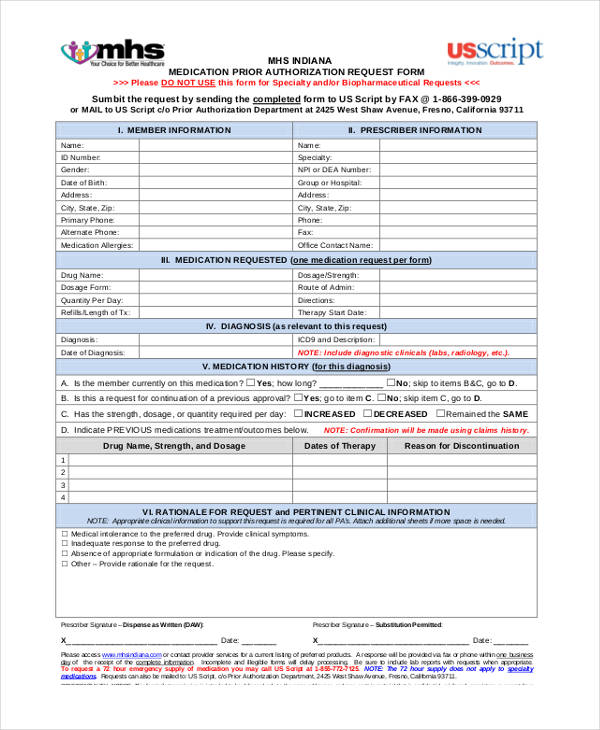
ads/responsive.txt Health Net Prior Authorization form for Medication
Contact name (first, last) member. Decisions & notification are made within 15calendar days* expedited request (md,. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Fast pass providers aren’t required to request prior authorization. Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans:
Hmsa Medicaid Form Request Fill Online, Printable, Fillable, Blank
_ patient information last name first name phone number gender m f date of birth member id # (if known): Fast pass providers aren’t required to request prior authorization. Web standard request for medicare and medicaid plans: Web utilization management (um) department prior authorization request phone number: This patient’s benefit plan requires prior authorization for certain medications in order for.
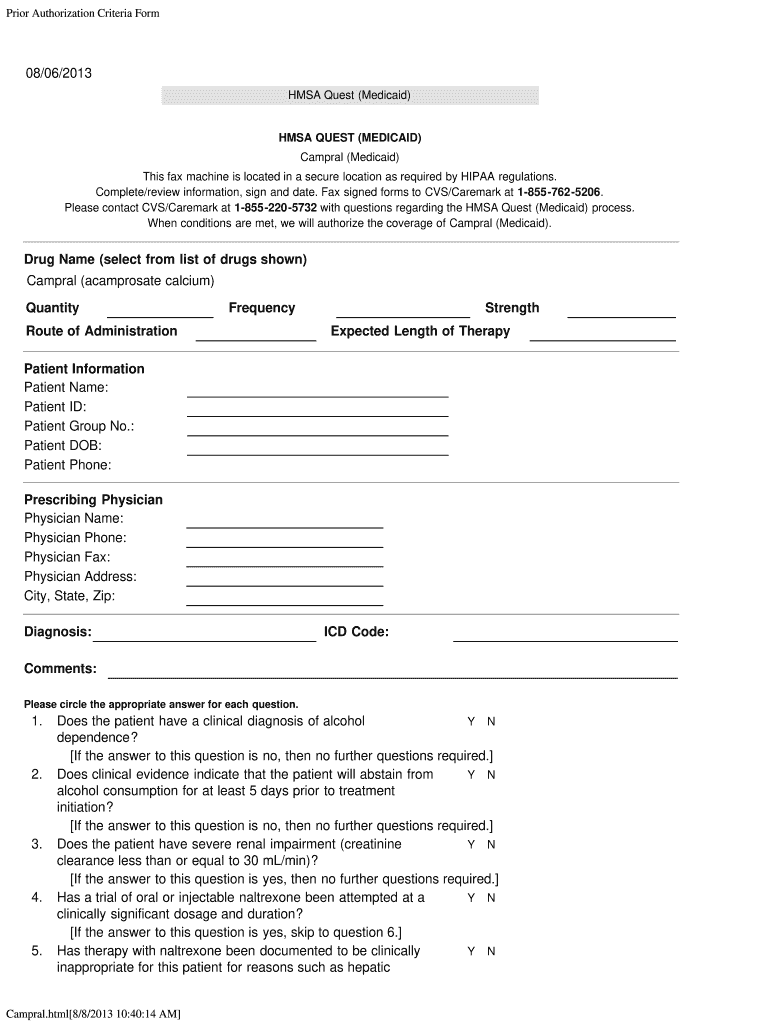
Authorization Medicaid Campral Fill Out and Sign Printable PDF
Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Contact name (first, last) member. Decisions & notification are made within.
Medco Prior Authorization Form Form Resume Examples XV8oMxYKzD
This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. To make an appropriate determination, providing the most accurate diagnosis for the use of the Web utilization management (um) department prior authorization request phone number: Decisions & notification are made within 15calendar days* expedited request (md,. Web this patient’s benefit plan requires.
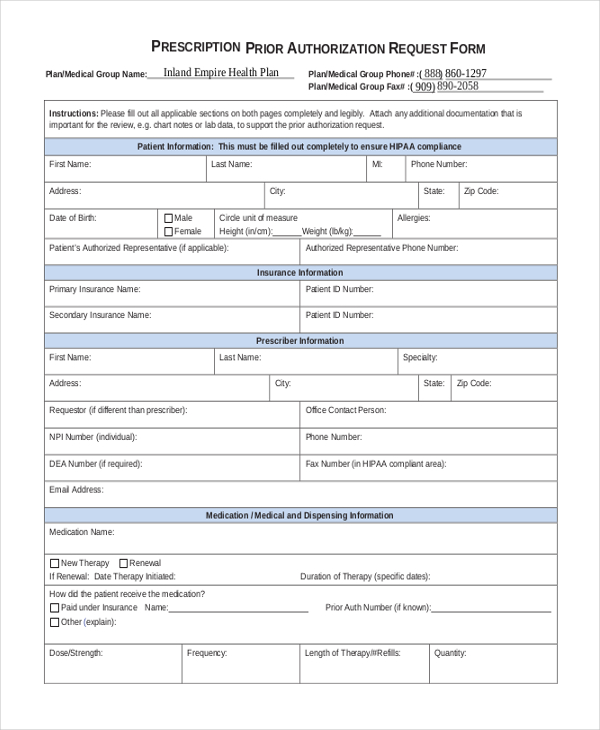
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Hmsa medical management department p. To.
Express Scripts Prior Authorization Form Medicare Part D Form
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Hmsa medical management department p. This standardized form is used for a general request for hmsa all lines of business when no.
Ach Payment Authorization Form Template Template 2 Resume Examples
Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. Contact name (first, last) member. Hmsa medical management department p. Web utilization management (um) department prior authorization request phone number: Decisions & notification are made within 15calendar days* expedited request (md,.
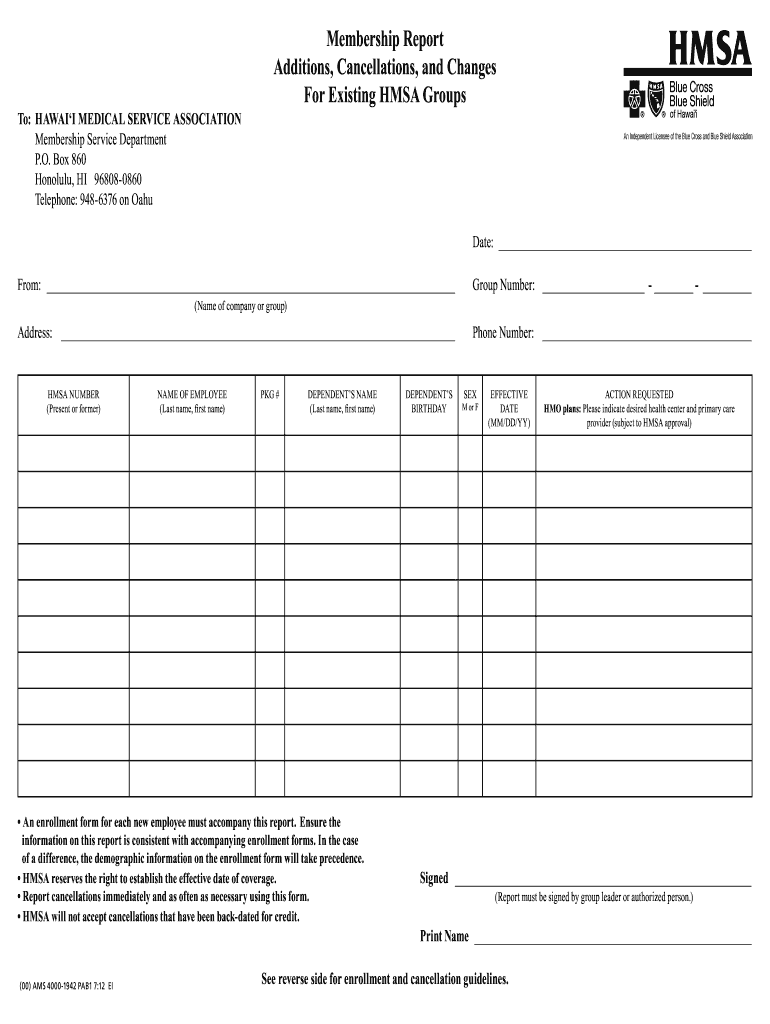
Hmsa Membership Report Form Fill Out and Sign Printable PDF Template
This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Hmsa medical management department p. Decisions & notification are made within 15calendar days* expedited request (md,. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans,.
FREE 13+ Prior Authorization Forms in PDF MS Word
Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date: To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web utilization management (um) department prior authorization request phone number: _ patient information last name first name phone number gender m f date of birth member.
Web Hawaii Medicaid Prior Authorization Form Hawaii Standardized Prescription Drug Prior Authorization Form* Request Date:
This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. _ patient information last name first name phone number gender m f date of birth member id # (if known): Web standard request for medicare and medicaid plans: Fast pass providers aren’t required to request prior authorization.
This Patient’s Benefit Plan Requires Prior Authorization For Certain Medications In Order For The Drug To Be Covered.
Contact name (first, last) member. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. To make an appropriate determination, providing the most accurate diagnosis for the use of the Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans:
Web This Patient’s Benefit Plan Requires Prior Authorization For Certain Medications In Order For The Drug To Be Covered.
Decisions & notification are made within 15calendar days* expedited request (md,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. Web utilization management (um) department prior authorization request phone number:
Web This Standardized Prior Authorization Request Form Can Be Used For Most Prior Authorization Requests And Use Across All Four Health Plans, Including Alohacare, Hmsa, 'Ohana Health Plan, And United Healthcare.
Hmsa medical management department p.