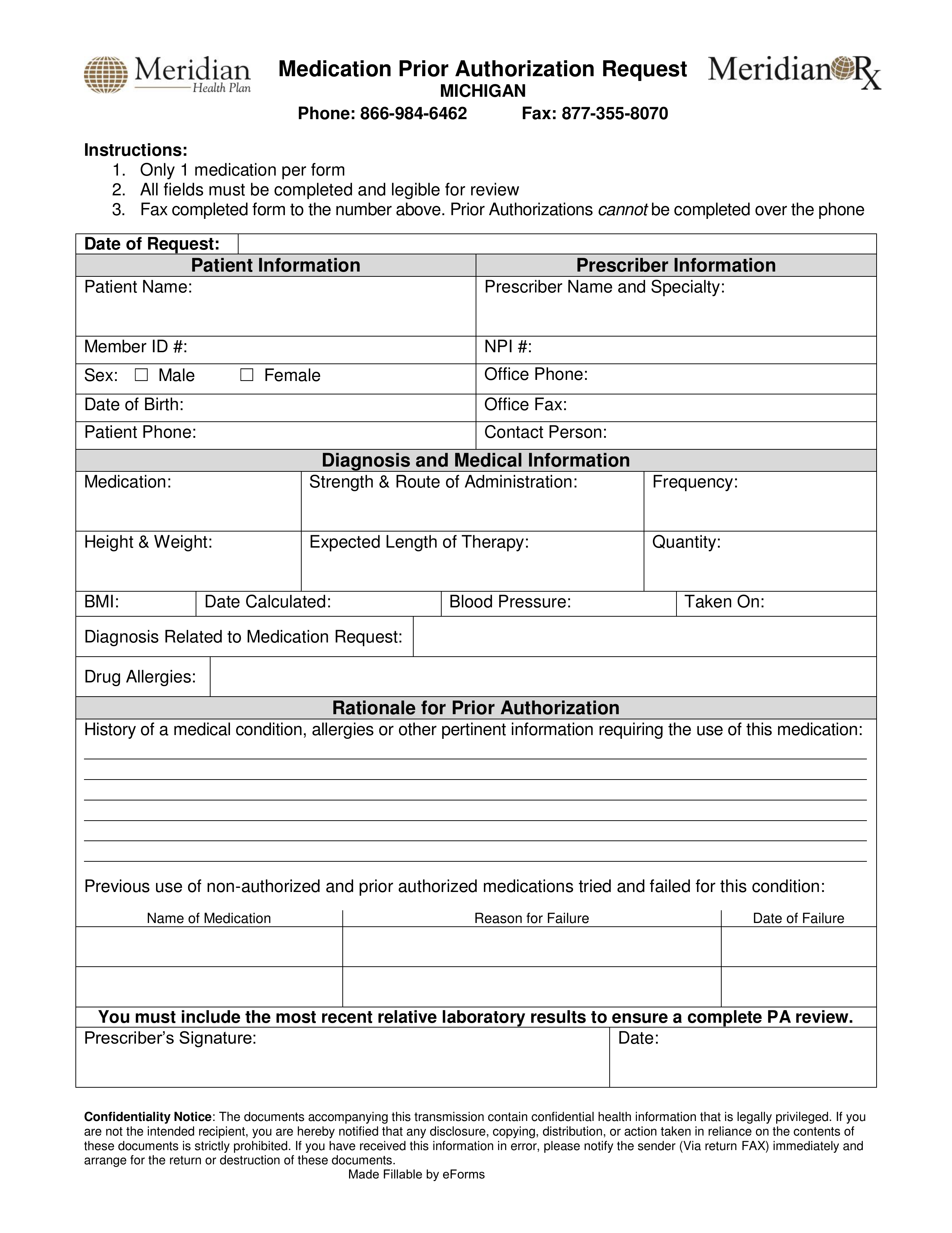
Meridian Prior Authorization Form
Meridian Prior Authorization Form - Prior authorizations cannot be submitted over the phone. You can get this document in spanish, or. To submit electronically, go to. You do not need a paper referral from meridian to see a. Login here to submit an authorization Musculoskeletal services procedures need to be verified by turningpoint. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web once you have created an account, you can use the meridian provider portal to: Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Web meridiancomplete is a health plan that contracts with both medicare and illinois medicaid to provide benefits of both programs to enrollees.
You can get this document in spanish, or. Web once you have created an account, you can use the meridian provider portal to: Learn more at ambetter from meridian. Web meridiancomplete is a health plan that contracts with both medicare and illinois medicaid to provide benefits of both programs to enrollees. Web prior authorization form standard/urgent requests: Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Musculoskeletal services procedures need to be verified by turningpoint. Login here to submit an authorization Use the meridian tool to see if a pre. Web 2022 information 2023 information submit a prior authorization for medical professional use only prior authorization instructions for meridiancomplete.
Prior authorizations cannot be submitted over the phone. Behavioral health discharge transition of care. Web this service requires prior authorization. Web meridiancomplete is a health plan that contracts with both medicare and illinois medicaid to provide benefits of both programs to enrollees. Only 1 medication per form all fields must be completed and legible for review. Musculoskeletal services procedures need to be verified by turningpoint. To submit electronically, go to. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Tools and resources specific clinical criteria available within the information linked below:
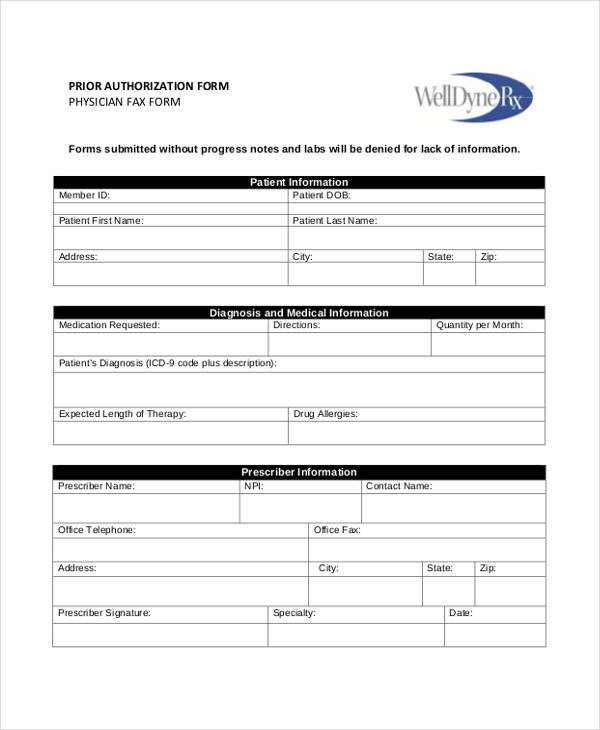
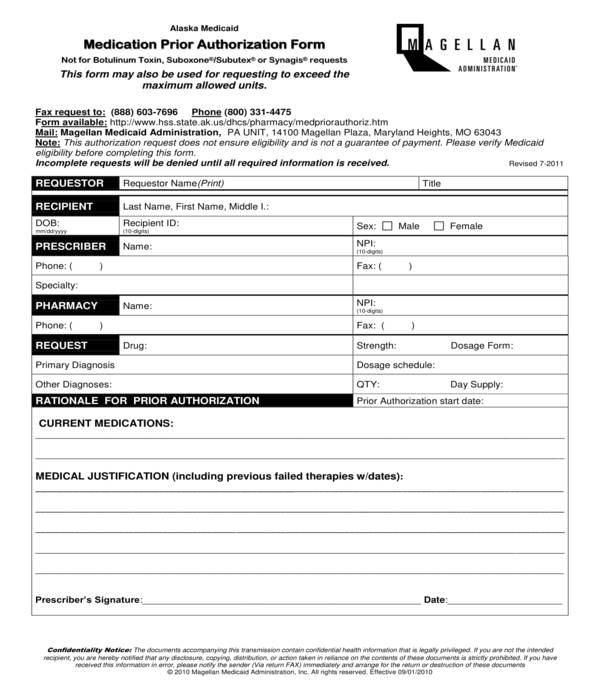
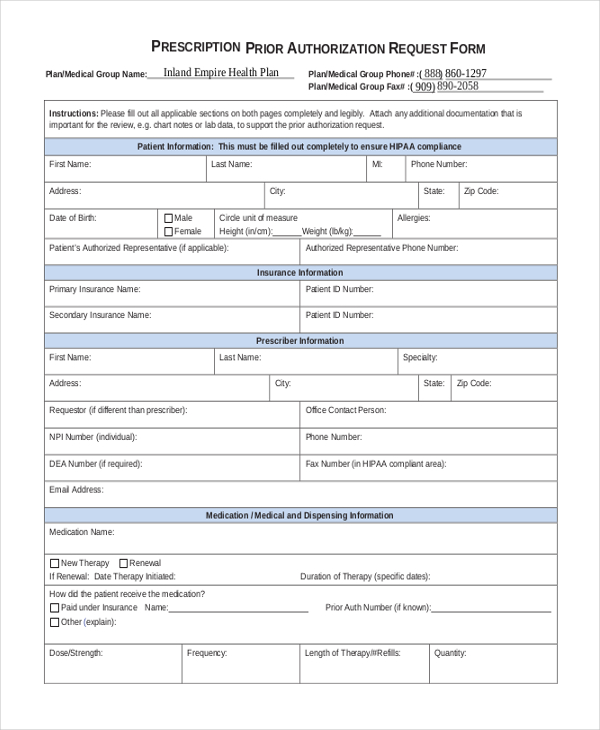
FREE 13+ Prior Authorization Forms in PDF MS Word
Prior authorizations cannot be submitted over the phone. Musculoskeletal services procedures need to be verified by turningpoint. Login here to submit an authorization Only 1 medication per form all fields must be completed and legible for review. Web yes no to submit a prior authorization login here.
What Is The Best Medicare Plan In Michigan
Behavioral health discharge transition of care. Web inpatient prior authorization form (pdf) outpatient prior authorization form (pdf) mental health forms: Prior authorizations cannot be submitted over the phone. Web this service requires prior authorization. Web yes no to submit a prior authorization login here.
FREE 11+ Prior Authorization Forms in PDF MS Word
Web meridiancomplete is a health plan that contracts with both medicare and illinois medicaid to provide benefits of both programs to enrollees. Web yes no to submit a prior authorization login here. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
To submit electronically, go to. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Use the meridian tool to see if a pre. You can get this document in spanish, or. Prior authorizations cannot be submitted over the phone.
Provider Service Area MeridianHealth of Michigan
Musculoskeletal services procedures need to be verified by turningpoint. Learn more at ambetter from meridian. Web once you have created an account, you can use the meridian provider portal to: Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Web this service requires prior authorization.
2018 Rate Hikes Michigan Early Look Aca Signups
Tools and resources specific clinical criteria available within the information linked below: Prior authorizations cannot be submitted over the phone. Web yes no to submit a prior authorization login here. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical.
Free Meridian Prior (Rx) Authorization Form PDF eForms
Behavioral health discharge transition of care. Web obtain a prior authorization from nia for an outpatient advanced imaging service. Musculoskeletal services procedures need to be verified by turningpoint. Web meridiancomplete is a health plan that contracts with both medicare and illinois medicaid to provide benefits of both programs to enrollees. Only 1 medication per form all fields must be completed.
Meridian Health Plan Illinois
To submit electronically, go to. Web inpatient prior authorization form (pdf) outpatient prior authorization form (pdf) mental health forms: You do not need a paper referral from meridian to see a. Musculoskeletal services procedures need to be verified by turningpoint. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy:
Bcbs Prior Authorization Form Alabama Form Resume Examples 5xm1e7r3rL
Web inpatient prior authorization form (pdf) outpatient prior authorization form (pdf) mental health forms: Web yes no to submit a prior authorization login here. Prior authorizations cannot be submitted over the phone. You do not need a paper referral from meridian to see a. Web obtain a prior authorization from nia for an outpatient advanced imaging service.
Michigan Information Meridian
Prior authorizations cannot be submitted over the phone. Learn more at ambetter from meridian. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web prior authorization form buy & bill drug requests:
You Can Get This Document In Spanish, Or.
Web 2022 information 2023 information submit a prior authorization for medical professional use only prior authorization instructions for meridiancomplete. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Musculoskeletal services procedures need to be verified by turningpoint. Prior authorizations cannot be submitted over the phone.
Web Obtain A Prior Authorization From Nia For An Outpatient Advanced Imaging Service.
Web meridian medicaid medical records. Login here to submit an authorization Web prior authorization form buy & bill drug requests: Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy:
Web Meridiancomplete Is A Health Plan That Contracts With Both Medicare And Illinois Medicaid To Provide Benefits Of Both Programs To Enrollees.
Tools and resources specific clinical criteria available within the information linked below: You do not need a paper referral from meridian to see a. Web once you have created an account, you can use the meridian provider portal to: Web prior authorization form standard/urgent requests:
Behavioral Health Discharge Transition Of Care.
Learn more at ambetter from meridian. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Use the meridian tool to see if a pre. Only 1 medication per form all fields must be completed and legible for review.