Unicare Prior Authorization Form
Unicare Prior Authorization Form - If the following information is not complete, correct, or legible, the pa process may be delayed. Web you can use the prior authorization form to submit a prior authorization request to unicare for review, but you will still need to submit the appropriate unicare precertification worksheet to provide the necessary clinical documentation to support the request. Requests may be submitted via the icr at availity.com.* Unicare will continue to review oncology specialty drugs. Web update to prior authorization process for medical specialty drug review. Save or instantly send your ready documents. Unicare is a pdp plan with a medicare contract. There are changes to the prior authorization process for unicare’s medical specialty drug review. Wait in a petient way for the upload of your unicare prior authorization. * availity, llc is an independent company providing administrative support services on behalf of unicare health plan of west virginia, inc.
Web update to prior authorization process for medical specialty drug review. Hit the get form button on this page. Select auth/referral inquiry or authorizations. If the following information is not complete, correct, or legible, the pa process may be delayed. Coverage is provided by unicare life & health insurance company. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. You can erase, text, sign or highlight as what you want. There are changes to the prior authorization process for unicare’s medical specialty drug review. Unicare is a pdp plan with a medicare contract. Requests may be submitted via the icr at availity.com.*
Easily fill out pdf blank, edit, and sign them. Wait in a petient way for the upload of your unicare prior authorization. Web services requiring prior authorization. Unicare is a pdp plan with a medicare contract. Requests may be submitted via the icr at availity.com.* Select auth/referral inquiry or authorizations. Member eligibility & benefits reports From the availity home page, select patient registration from the top navigation. Hit the get form button on this page. There are changes to the prior authorization process for unicare’s medical specialty drug review.
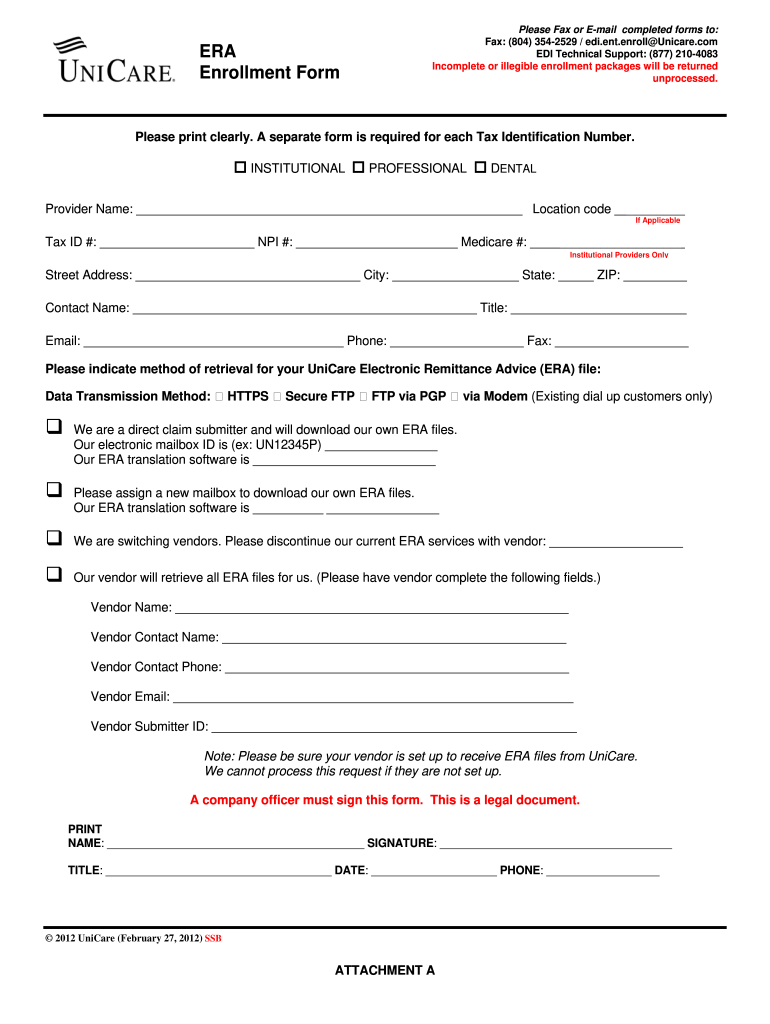
Unicare Eft Enrollment Form Fill Online, Printable, Fillable, Blank
Save or instantly send your ready documents. If the following information is not complete, correct, or legible, the pa process may be delayed. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. Unicare will continue to review oncology specialty drugs. Web update to prior authorization process for medical specialty drug review.
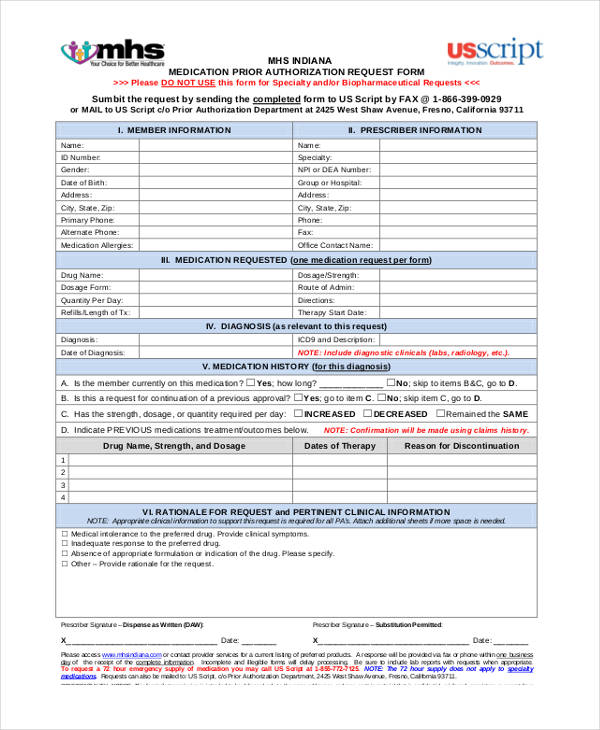
FREE 13+ Prior Authorization Forms in PDF MS Word
Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. From the availity home page, select patient registration from the top navigation. There are changes to the prior authorization process for unicare’s medical specialty drug review. Wait in a petient way for the upload of your unicare prior authorization. Unicare will continue to review.
Prior Authorization Form For Medicare Advantage Universal Network
You can also refer to the provider manual for information related to. Save or instantly send your ready documents. Coverage is provided by unicare life & health insurance company. Web update to prior authorization process for medical specialty drug review. There are changes to the prior authorization process for unicare’s medical specialty drug review.
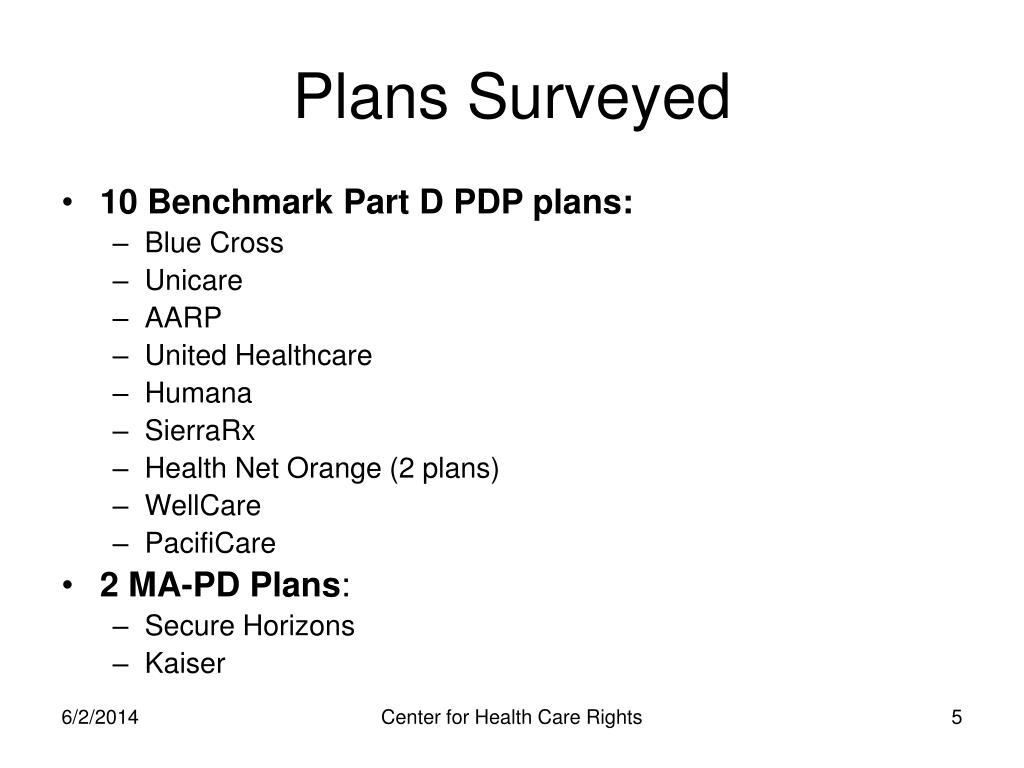
PPT Medicare Part D Transition, Prior Authorization, & Exceptions
Unicare will continue to review oncology specialty drugs. Coverage is provided by unicare life & health insurance company. Requests may be submitted via the icr at availity.com.* * availity, llc is an independent company providing administrative support services on behalf of unicare health plan of west virginia, inc. Web complete unicare prior authorization online with us legal forms.
Unicare Authorization Request Form Fill Online, Printable, Fillable
Web unicare health plan of west virginia, inc. You can erase, text, sign or highlight as what you want. You can also refer to the provider manual for information related to. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. There are changes to the prior authorization process for unicare’s medical specialty drug.
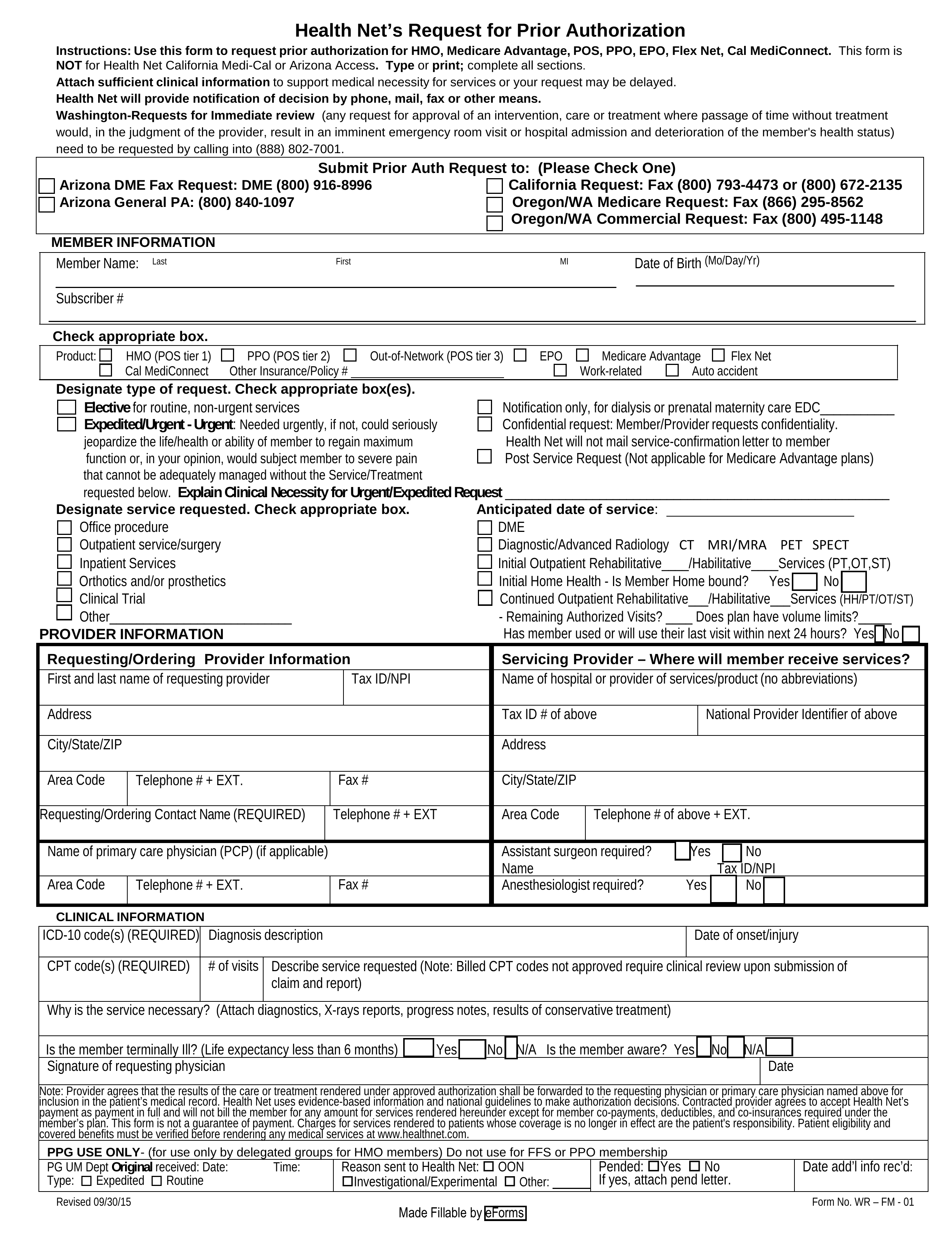
Free Health Net Prior (Rx) Authorization Form PDF eForms
Unicare will continue to review oncology specialty drugs. Coverage is provided by unicare life & health insurance company. There are changes to the prior authorization process for unicare’s medical specialty drug review. Web update to prior authorization process for medical specialty drug review. Requests may be submitted via the icr at availity.com.*
Bcbs Prior Authorization Form Michigan Form Resume Examples kDp3Og030Q
Save or instantly send your ready documents. If the following information is not complete, correct, or legible, the pa process may be delayed. Requests may be submitted via the icr at availity.com.* From the availity home page, select patient registration from the top navigation. Select auth/referral inquiry or authorizations.
Ach Payment Authorization Form Template Template 2 Resume Examples
* availity, llc is an independent company providing administrative support services on behalf of unicare health plan of west virginia, inc. Save or instantly send your ready documents. If the following information is not complete, correct, or legible, the pa process may be delayed. Coverage is provided by unicare life & health insurance company. You can erase, text, sign or.
FREE 41+ Authorization Forms in PDF Excel MS word
Coverage is provided by unicare life & health insurance company. Unicare will continue to review oncology specialty drugs. Enrollment in unicare depends on contract renewal. Web you can use the prior authorization form to submit a prior authorization request to unicare for review, but you will still need to submit the appropriate unicare precertification worksheet to provide the necessary clinical.
Prior Authorization List OptumCare
* availity, llc is an independent company providing administrative support services on behalf of unicare health plan of west virginia, inc. Hit the get form button on this page. Web services requiring prior authorization. Web unicare health plan of west virginia, inc. Easily fill out pdf blank, edit, and sign them.
Web You Can Use The Prior Authorization Form To Submit A Prior Authorization Request To Unicare For Review, But You Will Still Need To Submit The Appropriate Unicare Precertification Worksheet To Provide The Necessary Clinical Documentation To Support The Request.
From the availity home page, select patient registration from the top navigation. Enrollment in unicare depends on contract renewal. Web services requiring prior authorization. Member eligibility & benefits reports
Web Update To Prior Authorization Process For Medical Specialty Drug Review.
If the following information is not complete, correct, or legible, the pa process may be delayed. Wait in a petient way for the upload of your unicare prior authorization. Easily fill out pdf blank, edit, and sign them. * availity, llc is an independent company providing administrative support services on behalf of unicare health plan of west virginia, inc.
You Can Also Refer To The Provider Manual For Information Related To.
Unicare is a pdp plan with a medicare contract. Requests may be submitted via the icr at availity.com.* Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. There are changes to the prior authorization process for unicare’s medical specialty drug review.
Coverage Is Provided By Unicare Life & Health Insurance Company.
You can erase, text, sign or highlight as what you want. Select auth/referral inquiry or authorizations. Unicare will continue to review oncology specialty drugs. Web unicare health plan of west virginia, inc.