Wellcare By Allwell Prior Authorization Form
Wellcare By Allwell Prior Authorization Form - Prior authorizations for musculoskeletal procedures should be verified by turningpoint. Prior authorization, step therapy, & quantity limitations; Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Hepatitis c treatment prior authorization request. A wellcare prior authorization form is a document used for requesting certain prescription drugs or. Pharmacy policies & forms coverage determinations and. Web prior authorization, step therapy, & quantity limitations; Web for information about prior authorization, please visit the authorization page. Web prior authorization, step therapy, & quantity limitations;
Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Login or create a secure portal account; Web providers must obtain prior authorization for certain services and procedures. Prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Prior authorization, step therapy, & quantity limitations; Web prior authorization, step therapy, & quantity limitations; Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service on or after 11/1/2022. Hospice information for medicare part d plans. Authorization requirements are available in the quick reference guide. If the planned admission date.
Prior authorizations for musculoskeletal procedures should be verified by turningpoint. 2022 allwell inpatient pa form (pdf). Pharmacy policies & forms coverage determinations and. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web prior authorization, step therapy, & quantity limitations; Web what is prior authorization? Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service on or after 11/1/2022. Web wellcare prior (rx) authorization form. Login or create a secure portal account;
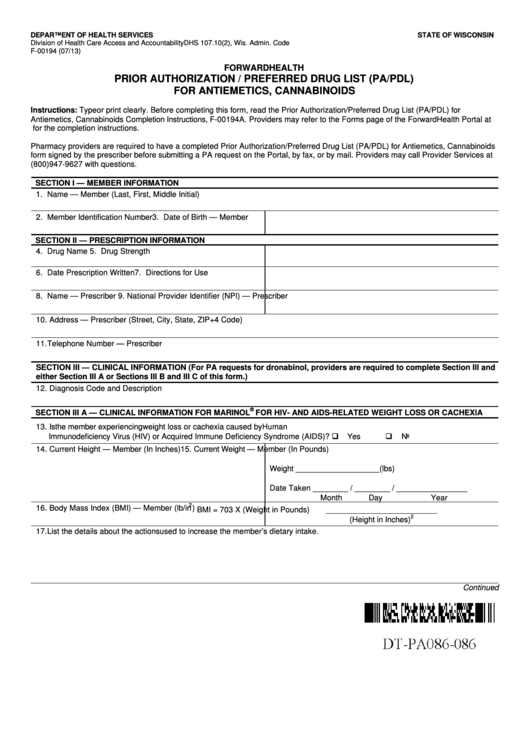
Prior Authorization / Preferred Drug List printable pdf download
Web wellcare prior (rx) authorization form. Web for information about prior authorization, please visit the authorization page. Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service on or after 11/1/2022. Web providers must obtain prior authorization for certain services and procedures. Web pharmacy policies & forms coverage determinations and.
Wellcare Part D Formulary 2023 2023
Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. If the planned admission date. Login or create a secure portal account; Web complex imaging, mra, mri, pet and ct scans need to be verified by nia. Web 2021 azch inpatient pa form (pdf).
Wellcare Medicaid Prior Authorization form Elegant 49 New
Web 2021 azch inpatient pa form (pdf) wellcare by allwell. Web authorization form request for additional units. We’ve combined multiple brands under. Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service on or after 11/1/2022. Login or create a secure portal account;
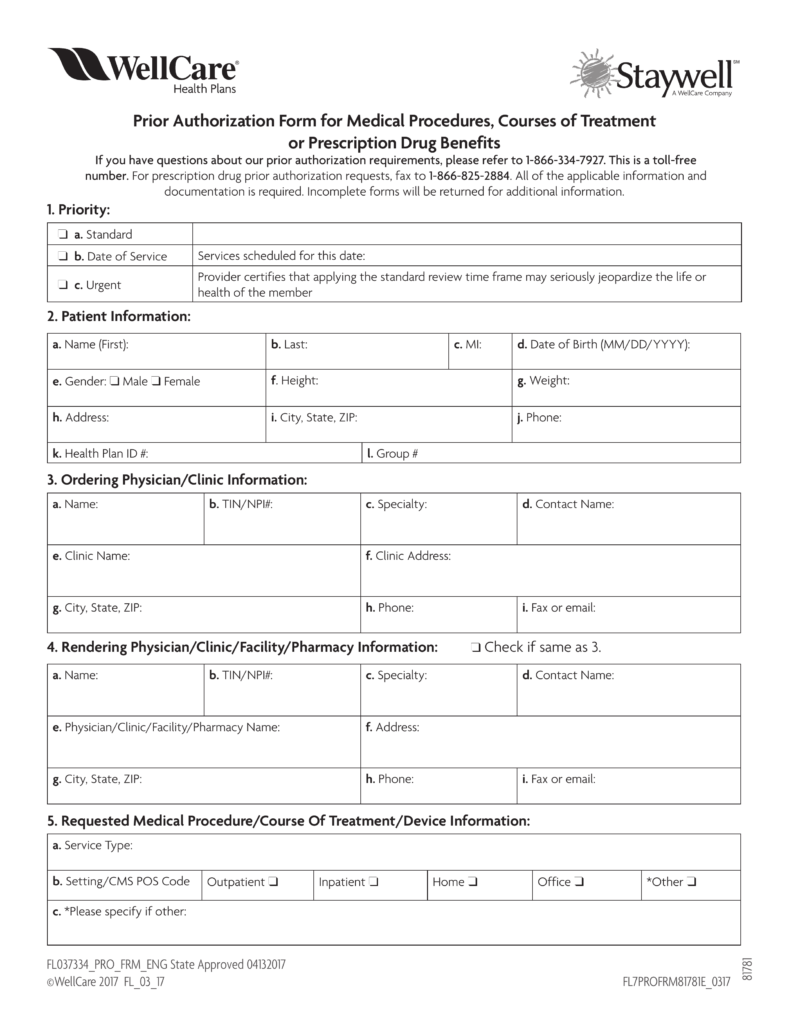
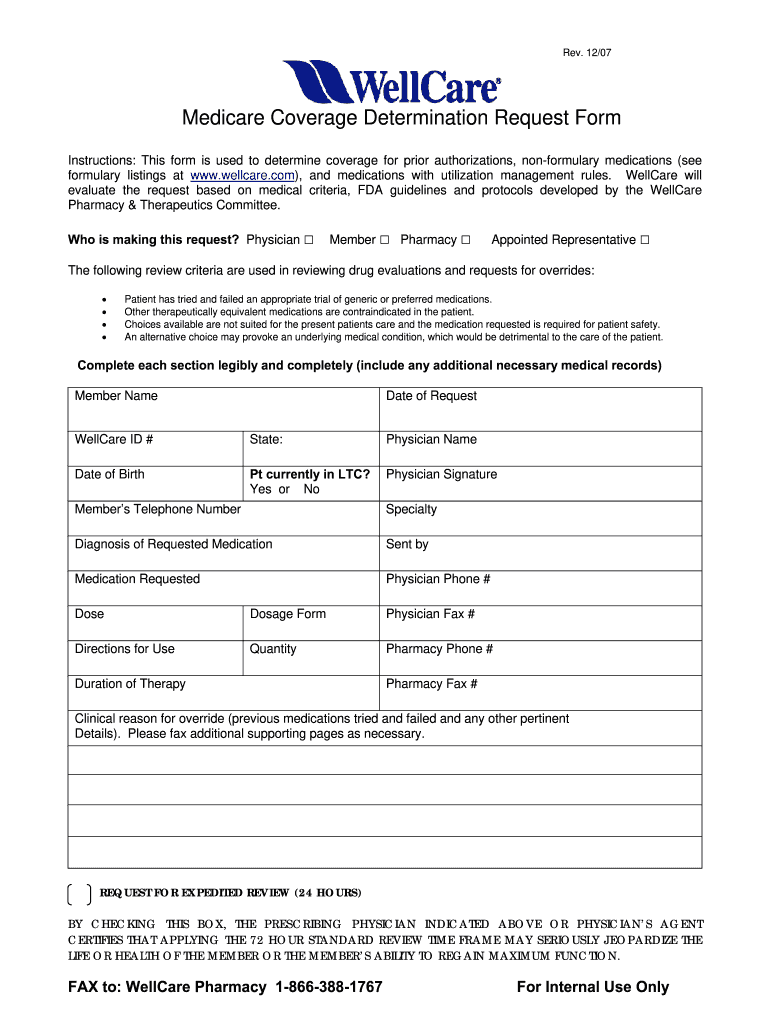
Free WellCare Prior (Rx) Authorization Form PDF eForms
Web authorization form request for additional units. Allwell from superior healthplan has some exciting changes to our medicare plans for 2022. Pharmacy policies & forms coverage determinations and. Web find out more about becoming a wellcare by allwell from mhs contracted provider. Prior authorizations for musculoskeletal procedures should be verified by turningpoint.
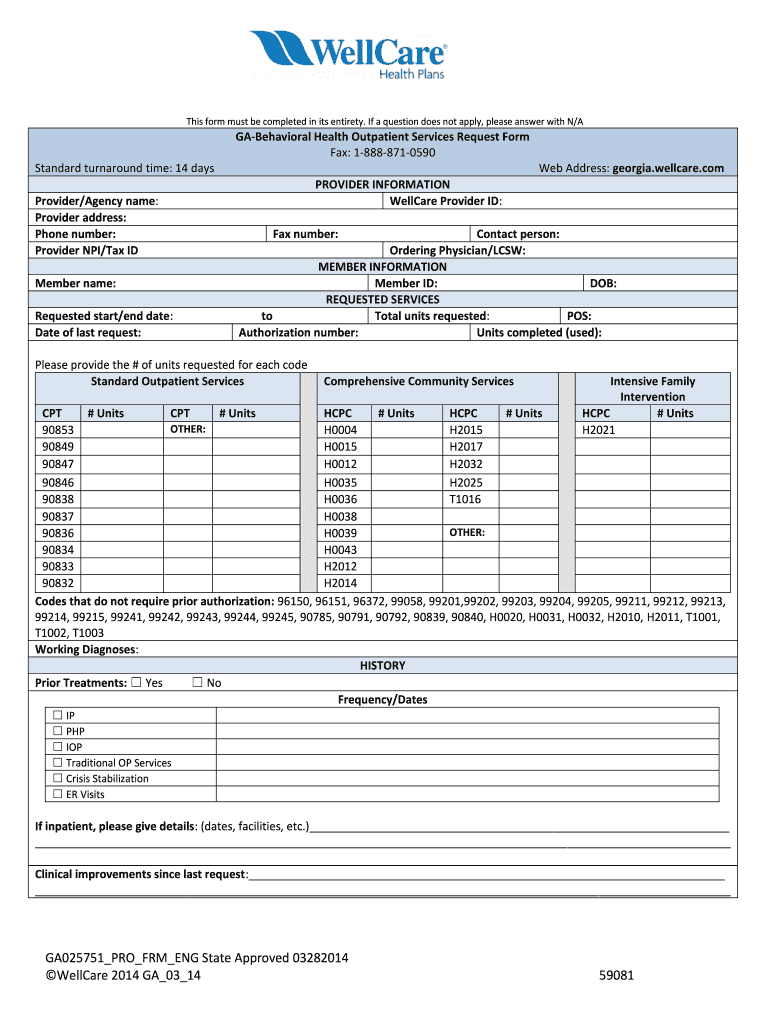
Wellcare Behavioral Health Service Request Form Fill Out and Sign
Prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Complex imaging, mra, mri, pet and ct scans need to be verified. Web what is prior authorization? Web complex imaging, mra, mri, pet and ct scans need to be verified by nia. Pharmacy policies & forms coverage determinations and.
Wellcare Drug Formulary 2023 2023 Calendar
Web providers must obtain prior authorization for certain services and procedures. Prior authorizations for musculoskeletal procedures should be verified by turningpoint. 2022 allwell inpatient pa form (pdf). Prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Allwell from superior healthplan has some exciting changes to our medicare plans for.
Wellcare Card 1 newacropol
Web authorization form request for additional units. Allwell from superior healthplan has some exciting changes to our medicare plans for 2022. Authorization requirements are available in the quick reference guide. Complex imaging, mra, mri, pet and ct scans need to be verified. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response.
Wellmed Prior Authorization Form Fill Online, Printable, Fillable
Web complex imaging, mra, mri, pet and ct scans need to be verified by nia. Web prior authorization, step therapy, & quantity limitations; Hepatitis c treatment prior authorization request. Pharmacy policies & forms coverage determinations and. Web prior authorization, step therapy, & quantity limitations;
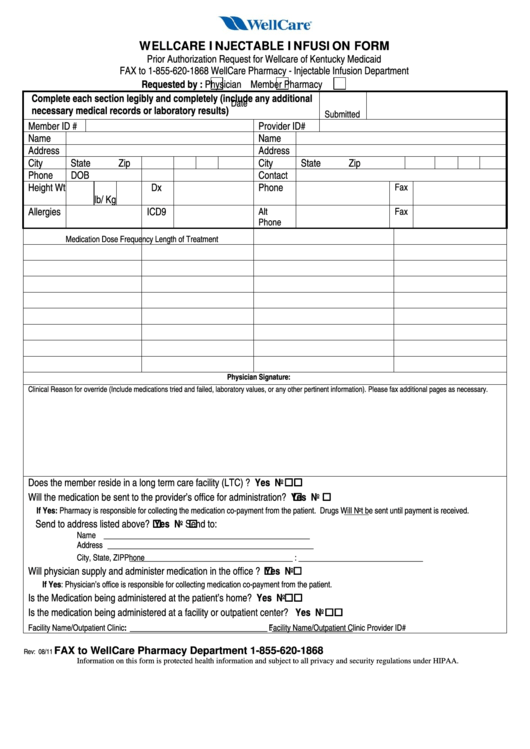
Fillable Wellcare Injectable Infusion Form Prior Authorization
Web prior authorization, step therapy, & quantity limitations; Web complex imaging, mra, mri, pet and ct scans need to be verified by nia. Authorization requirements are available in the quick reference guide. Pharmacy policies & forms coverage determinations and. Login or create a secure portal account;
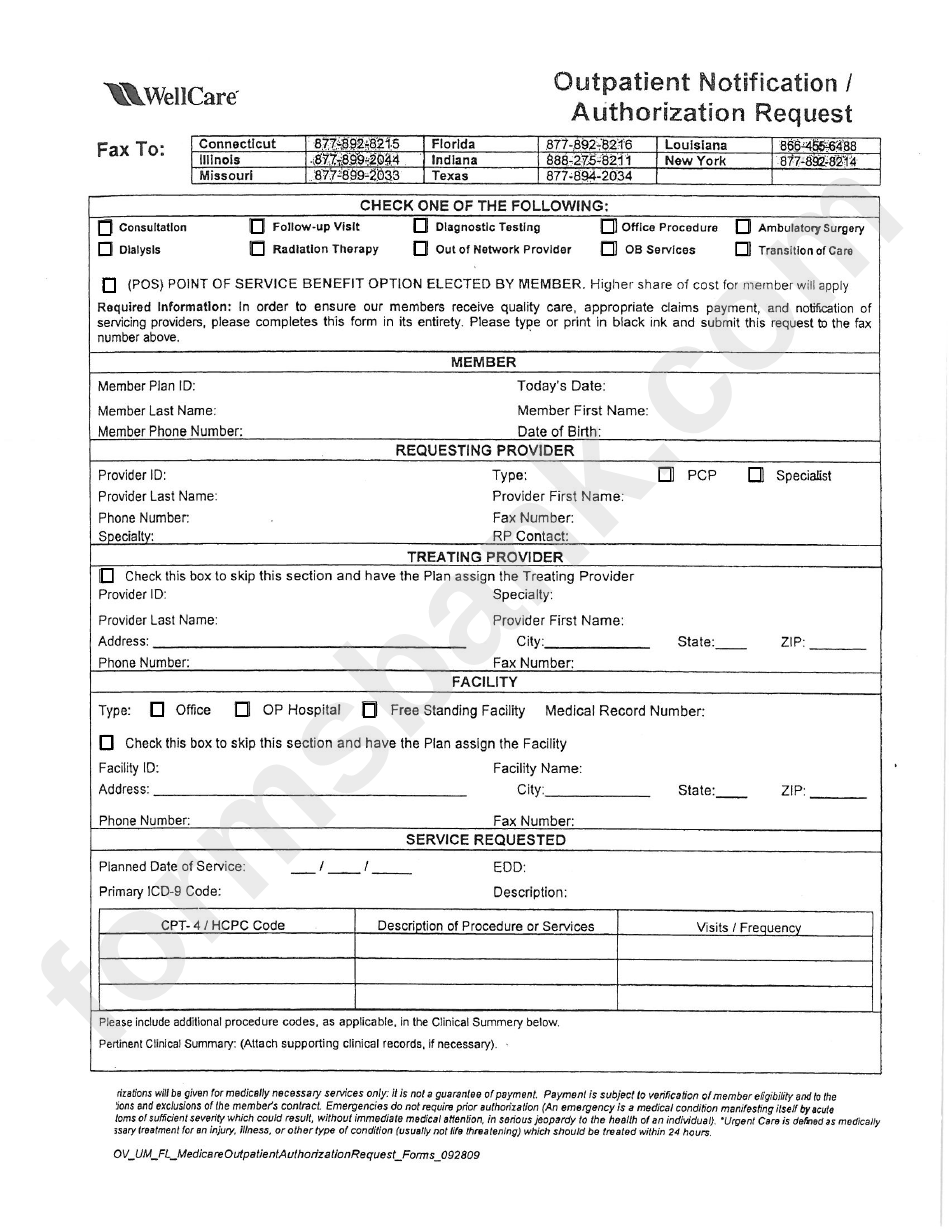
Fillable Outpatient Notification /authorization Request Wellcare
Complex imaging, mra, mri, pet and ct scans need to be verified. Web authorization form request for additional units. Pharmacy policies & forms coverage determinations and. 2022 allwell inpatient pa form (pdf). Web wellcare prior (rx) authorization form.
Hepatitis C Treatment Prior Authorization Request.
Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web pharmacy policies & forms coverage determinations and redeterminations; Prior authorization, step therapy, & quantity limitations; Web providers must obtain prior authorization for certain services and procedures.
Web What Is Prior Authorization?
Complex imaging, mra, mri, pet and ct scans need to be verified. Web authorization form request for additional units. Web prior authorization, step therapy, & quantity limitations; Pharmacy policies & forms coverage determinations and.
Login Or Create A Secure Portal Account;
Authorization requirements are available in the quick reference guide. Hospice information for medicare part d plans. A wellcare prior authorization form is a document used for requesting certain prescription drugs or. Pharmacy policies & forms coverage determinations and.
Prior Authorizations For Musculoskeletal Procedures Should Be Verified By Turningpoint.
Web find out more about becoming a wellcare by allwell from mhs contracted provider. Allwell from superior healthplan has some exciting changes to our medicare plans for 2022. Prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response.